INTRODUCTION
The Inflation Reduction Act of 2022 includes several provisions to lower prescription drug costs for people with Medicare and reduce drug spending by the federal government, including a number of changes to the Medicare Part D drug benefit. These changes include (a) a cap on out-of-pocket drug spending for seniors enrolled in Medicare Part D plans, and (b) requiring Part D plans and drug manufacturers to pay a greater share of costs for Part D enrollees with high drug costs.
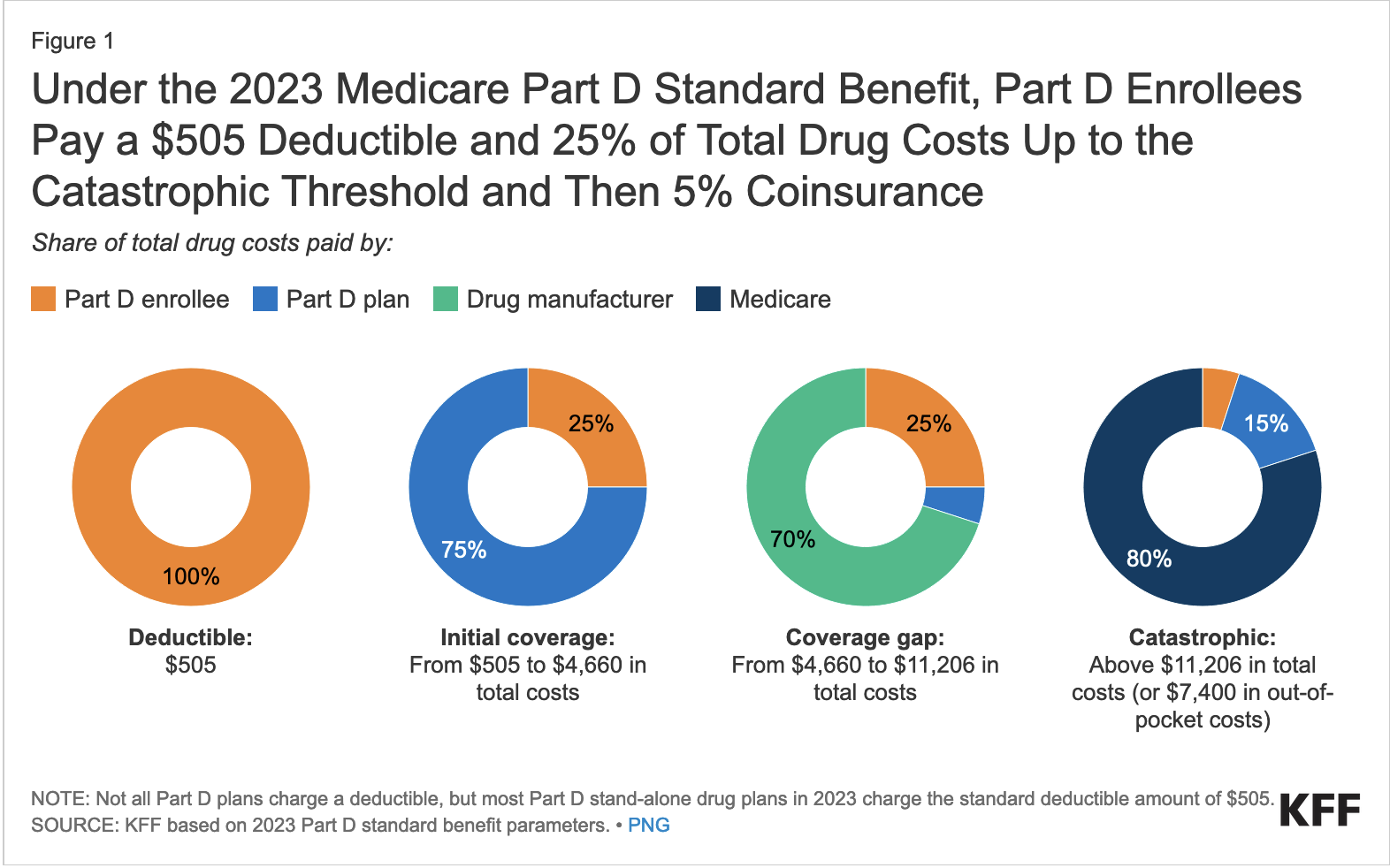
The chart below shows how Medicare Part D worked in 2023:
WHAT’S CHANGED IN 2024?
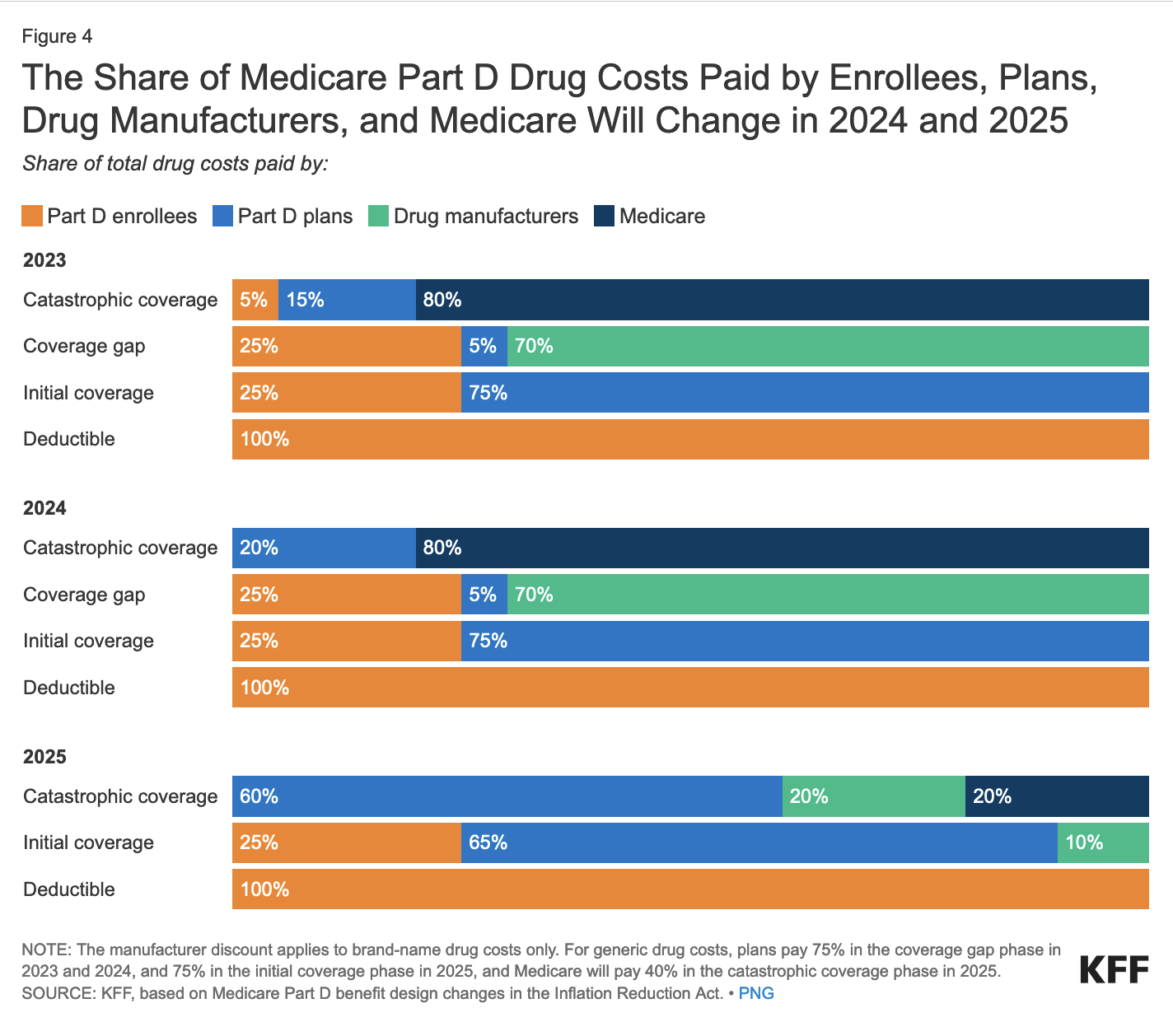
In 2024, costs in the catastrophic phase have changed: the 5% coinsurance requirement for Part D enrollees is eliminated, and Part D plans pay 20% of total drug costs in this phase, instead of 15%.
2024: Elimination of 5% Coinsurance for Part D
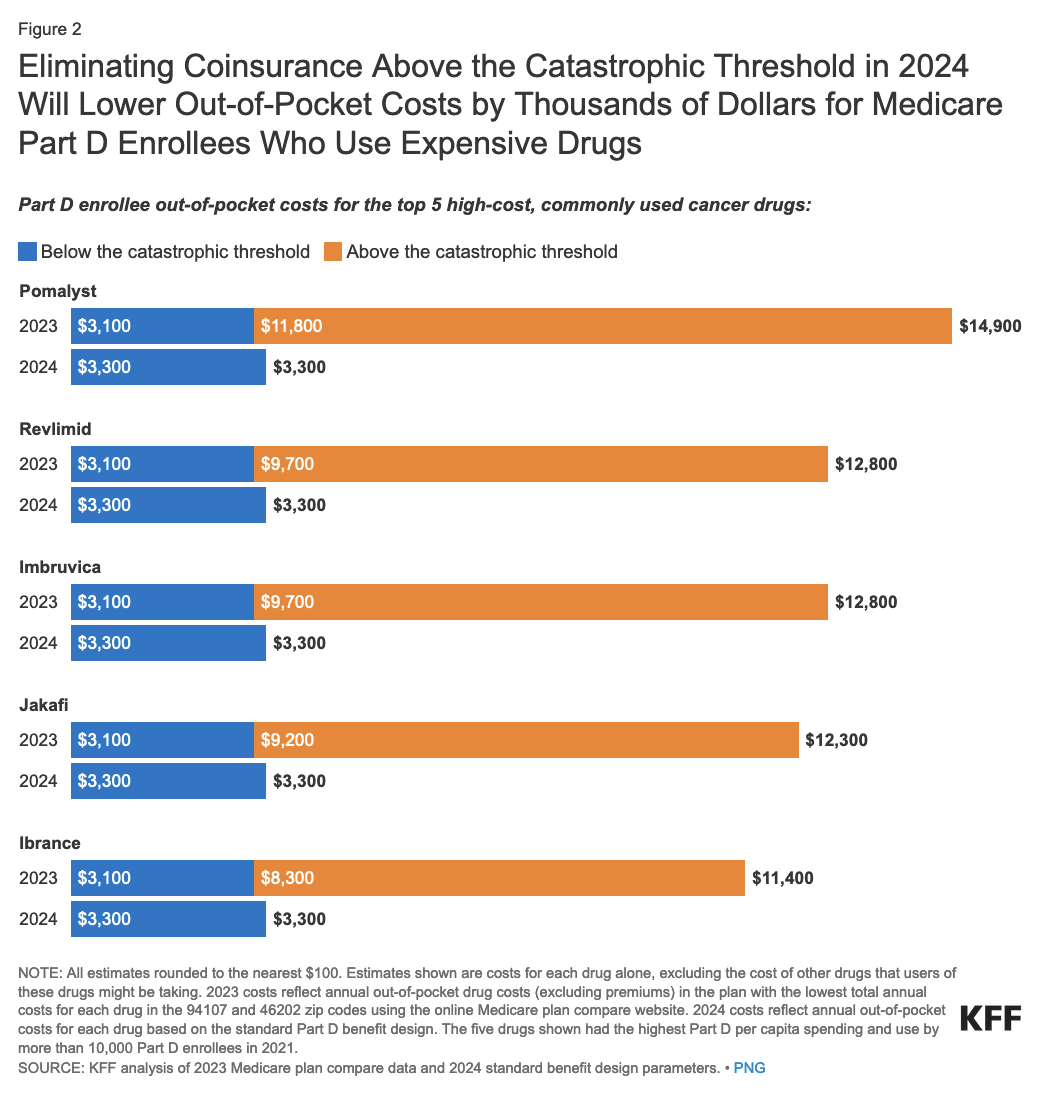
In 2024, once Part D enrollees without low-income subsidies (or “LIS”) spend enough on drugs to qualify for catastrophic coverage, they are longer required to pay 5% of their drug costs, effectively capping their out-of-pocket spending.
In 2024, the catastrophic threshold is set at $8,000. This amount includes what Part D enrollees spend out of pocket, plus the value of the manufacturer price discount on brands in the coverage gap phase. At this amount, Part D enrollees who take only brand-name drugs in 2024 will spend about $3,300 out of their own pockets, but won’t face additional costs for their medications.
2024: Part D Plans Pay Larger Share
With the elimination of the 5% coinsurance requirement for Part D enrollees in the catastrophic coverage phase, Part D plans are required to pay 20% of total drug costs in this phase in 2024, up from 15% in 2023 and prior years.
WHAT WILL CHANGE IN 2025?
Changes in 2025 include:
- a new $2,000 out-of-pocket spending cap,
- elimination of the coverage gap phase,
- a higher share of drug costs paid by Part D plans in the catastrophic phase, along with a new manufacturer price discount and reduced liability for Medicare in this phase, and
- changes to plan costs and the manufacturer price discount in the initial coverage phase.
2025: Out-of-pocket drug spending will be capped at $2,000
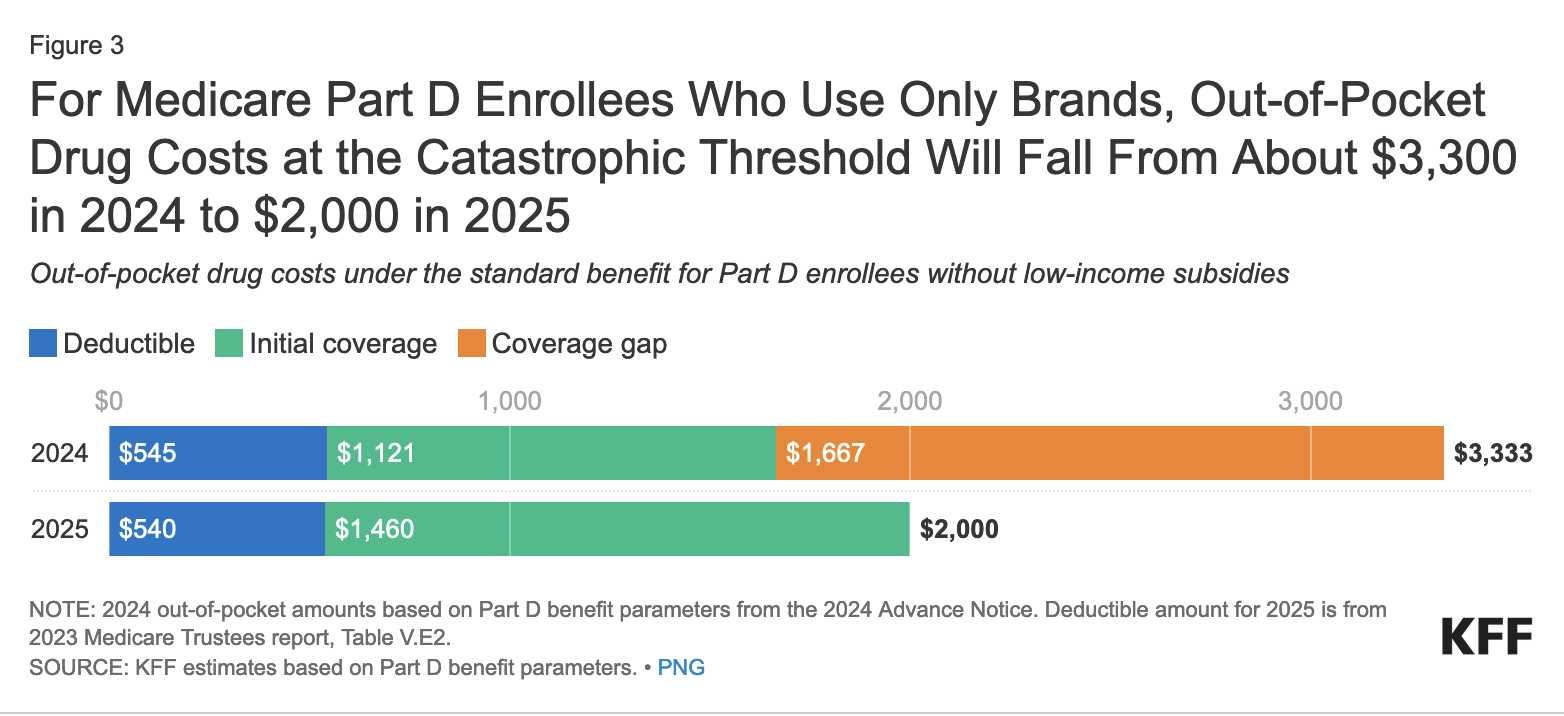
Beginning in 2025, Part D subscribers’ out-of-pocket drug costs will be capped at $2,000. This amount will be indexed to rise each year after 2025 at the rate of growth in per capita Part D costs. This cap does not apply to out-of-pocket spending on Part B drugs.
For Part D plan subscribers who take only brand-name drugs, annual out-of-pocket costs at the catastrophic threshold will fall from around $3,300 in 2024 to $2,000 in 2025 (see chart below). As a result, Part D subscribers on brand-name drugs who have drug costs high enough to reach the catastrophic threshold could save about $1,300 in 2025 compared to what they would spend in 2024.
2025: The coverage gap phase will be eliminated
The coverage gap phase, where Part D enrollees had faced 100% of their total drug costs under the original Part D benefit design and currently face 25% of costs for brand-name and generic drugs, will be eliminated in 2025.
This means that Part D enrollees will no longer face a change in their cost sharing for a given drug when they move from the initial coverage phase to the coverage gap phase, which is the case in most Part D plans today, since most plans charge varying cost-sharing amounts, rather than the standard 25% coinsurance, in the initial coverage phase.
2025: Part D plans and drug manufacturers will pay a larger share of costs for catastrophic coverage, and Medicare will pay a smaller share
Medicare’s share of total costs in the catastrophic phase (reinsurance) will decrease from 80% to 20% for brand-name drugs and from 80% to 40% for generic drugs beginning in 2025.
This reduction will help address concerns about the substantial increase in Medicare’s reinsurance payments to Part D plans over time, which accounted for close to half (48%) of total Part D spending in 2022, up from 14% in 2006, based on data from the Medicare Trustees 2023 annual report.
Medicare Part D plans’ share of costs will increase from 15% to 60% for both brand-name and generic drugs above the cap, and drug manufacturers will be required to provide a 20% price discount on brand-name drugs.
WHAT OTHER CHANGES ARE BEING MADE TO PART D?
As of 2023, the out-of-pocket cost of insulin products is limited to no more than $35 per month in all Part D plans. In addition, adult vaccines covered under Part D, such as the shingles vaccine, are covered with no cost sharing.
Starting in 2024, people with Medicare who have incomes up to 150% of the poverty level, and resources at or below the limits for partial low-income subsidy benefits, will be eligible for full benefits under the Part D Low-Income Subsidy (“LIS”) Program. The law eliminates the partial LIS benefit currently in place for individuals with incomes between 135% and 150% of the poverty level.
Also starting in 2024, the calculation of the base beneficiary premium will be adjusted, as needed, to limit increases in the base premium to no more than 6% from the prior year. Premiums for individual Part D plan premiums and annual plan-level premium increases will continue to vary, however.
Starting in 2025, Part D enrollees will have the option of spreading out their out-of-pocket costs over the year rather than face high out-of-pocket costs in any given month.
Data and images courtesy of Kaiser Family Foundation (https://kff.org)
Contact us today to learn more about health insurance before retirement, Medicare, and robust retirement planning.
PLEASE SEE important disclosure information at springwaterwealth.com/blog-disclosure/.
